Most athletes have experienced some type of tendon injury during their athletic career and can relate to the familiar ache or pain associated with ‘tendonitis.” Tendon pain usually lingers for quite some time and they are also frequently recurrent, putting a significant damper on your ability to train consistently.
Now the following explanation about tendon injuries might seem like a grad school class in biomechanics, but bear with me, it is worth your time. The better you understand how tendons get injured, and what happens to them when they do, the easier it is to fix them.
What is Tendinopathy?
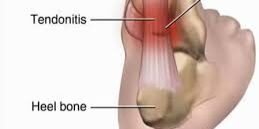
If you have been in athletics long enough, you have likely heard of the term “tendonitis” when describing tendon pain. Unfortunately, the labeling of this pain is incorrect. The term “itis” is used to describe inflammation, and implies an inflammatory problem. However, research over the past 10 years clearly shows that the problem is not an inflammatory issue, but is actually a breakdown of the tendon tissue.
We advocate the use of the term “tendinopathy” as a generic descriptor of the clinical conditions in and around tendons arising from “overuse.”
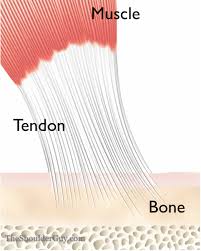
Evidence points towards a couple of reasons for tendinothapy, including (1) a biochemical cause of pain and (2) a breakdown of the collagen fibers that make up the tendon. Isolated inflammatory lesions are infrequent and are mostly associated with tendon ruptures. In general, tendinopathy can be viewed as a failure of the tendon tissue to adapt to the stresses placed on the tissue.
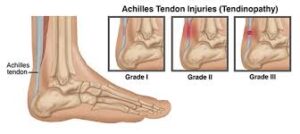
Three categories are used to describe the different stages of tendon injury, and each stage requires a slightly different approach to rehabilitation and outcome.
The 3 stages of tendon pathology are:
- Reactive tendinopathy
- Tendon dysrepair or failed healing
- Degenerative tendinopathy
Stage 1: Reactive Tendinopathy
Reactive tendinopathy occurs following acute tensile or compressive overloading to the tendon. In the early stages of tendinopathy, the cells are activated. This increase in cellular activity is responsible for increased water uptake in the tendon, which, in turn, makes the tendon look and feel a bit thicker. The purpose of this cellular response is to create a form of tissue adaptation that is designed to increase the cross-sectional area of the tendon. This increase in cross-sectional area decreases the force per unit area in the tendon and therefore reduces the stress placed on the tendon. In other words, the cellular response creates a temporary solution, a way to buffer the forces until long term changes in either tendon structure or mechanical properties can occur. The activated cells are responsible for producing chemicals, which trigger a pain response. If this process is not reversed, it will ultimately result in degeneration and weakening of the collagen fiber structure, which leads us into stage 2, the tendon disrepair/failed healing stage.
In summary, the reactive tendinopathy stage is a short-term adaption to tendon overload, which thickens the tendon, reduces stress and increases stiffness. The tendon has the potential to revert back to normal if the overloading is reduced or if there is sufficient time between loading sessions to allow for tendon adaption.
Stage 2: Tendon Disrepair
This is where tendon breakdown starts to occur. True damage to the tendon tissue is occurring. There is still no inflammation in the tendon but there has been enough cellular activation causing pain and fluid accumulation around the tendon that the structure of the collagen fiber has started to fail. Modifications to exercise activities and tendon loading need to occur in order to prevent tissue death from occurring.
Stage 3: Degenerative Tendinopathy
The third and final stage of tendon injury is called degenerative tendinopathy and it is in this stage that the tendon structure itself starts to change and includes areas of cell death. It should be noted that the whole tendon is not degenerated. In fact, it is more like small areas of degenerative tendon tissue surrounded by normal tendon and areas of tendon that are in other stages of pathology. Unfortunately, for the areas of tendon in the degenerative stage there is little capacity to recover due to the limited blood flow and length of time that stress and strain have been placed on that area of tendon. However, degenerative tendons can show improved function despite not returning to normal size or structure on imaging.
How do you Treat Tendinopathy?
In the early reactive phase, taking over the counter anti-inflammatory medication like ibuprofen has proven to be beneficial. I know, this sounds a little strange because we just said that tendons do not actually inflame BUT the anti-inflammatory properties in this medication can slow down the increased cellular activity, thereby decreasing the amount of pain producing chemicals in the tissue. Research shows that taking this as prescribed on the bottle for 1-2 weeks can help control symptoms of tendon pain.
Steroid injections should be used with caution. Steroids are a powerful anti-inflammatory for sure, but the side effects can be detrimental. Steroids have the potential to significantly decrease the strength of the tendon tissue, leaving it more vulnerable to complete tearing.
Corporal shock wave therapy, ultrasound, iontophoresis and laser therapy have not shown enough benefit in research studies and can therefore not be recommended for the treatment of tendinopathy.
Preliminary work with platelet rich plasma (PRP) injections and stem cells is promising but needs further research. This will be the topic of a blog in the very near future, so keep your eye out for that.
Friction massage has been proposed as an effective treatment in tendon injuries in the early stages of tendinopathy. The rational for this technique is that it helps improve tendon structure. However, there are few human studies to support this and the ones that have been performed show mixed results.
Recently, programs that use eccentric type exercises have shown to be successful. However, it is not known how exactly this affects the tendon healing process, and there is no consensus in the exact protocol that should be used.
How does Tendon Rehabilitation Work?
First and foremost the therapists at Mondo Sports Therapy will do a thorough evaluation to determine why the tendon is breaking down in the first place. It is very easy to say, “oh, my tendon flared up because I am running 50 miles a week.” Fair enough, but if it is just the running miles that matter, why is it that only your left Achilles tendon that hurts and not your right one, too? They run just as many miles!
Usually there is an underlying biomechanical deficit that caused the tendon to be overloaded. This biomechanical deficit is frequently a combination of joint restrictions and muscle imbalance. Biomechanical deficits are treated with joint mobilizations, soft tissue work, and appropriate exercises.
As far as the exercises are concerned, it is vital to find the baseline training level that does not provoke the tendon and use this as the point to start the rehab process.
In the clinic, we find the precise loading tension that a tendon can tolerate. We then design an exercise program that is heavy on low loading, high repetition type activities. In time, we add higher level loading activities, including plyometrics, and a return to running program.
The Alter G is an extremely useful piece of equipment in the tendon healing process. This is a body-weight assisted treadmill, which means you can run without putting too much stress on the symptomatic tendon. We are one of very few facilities in Austin that has one and it is used extensively in tendon rehab. For more information about body weight assisted running, check the Alter G section on our website.
We usually see our patients once a week for physical therapy, but you will be doing prescribed exercises on your own 5 days a week.
How Long Will it Take Before I am Better?
Since the metabolism of the tendon is low, the healing process takes time. If the tendon is in the early, reactive phase, we should be able to get a handle on the symptoms within 2-3 weeks. However, if the tendon problem has progressed to the degenerative phase, where significant breakdown of tendon tissue has occurred, the recovery time can take 6-12 months.
Can I Run While I Rehab From a Tendon Problem?
It all depends on the amount of pain, and what stage of the tendinopathy process you are in. We use three baseline parameters when it comes to judging if you can run with this injury or not:
1. No pain > 2 or 3 on a scale from 0-10
2. No limping while you run
3. No increased pain for longer than 30 minutes after you are done running
If you stay within those parameters, you should progress. However, if you ignore them, then you are likely putting more stress on the tissue than it can tolerate and are, in essence, causing more tissue damage, thereby prolonging the healing process.
Keep in mind that there are no magic fixes when it comes to tendon healing. It comes down to long, arduous work, but tendons are living tissue, which means they will heal if you do the right thing.
If you have any questions at all, the physical therapists at Mondo Sports Therapy will happily address them for you.